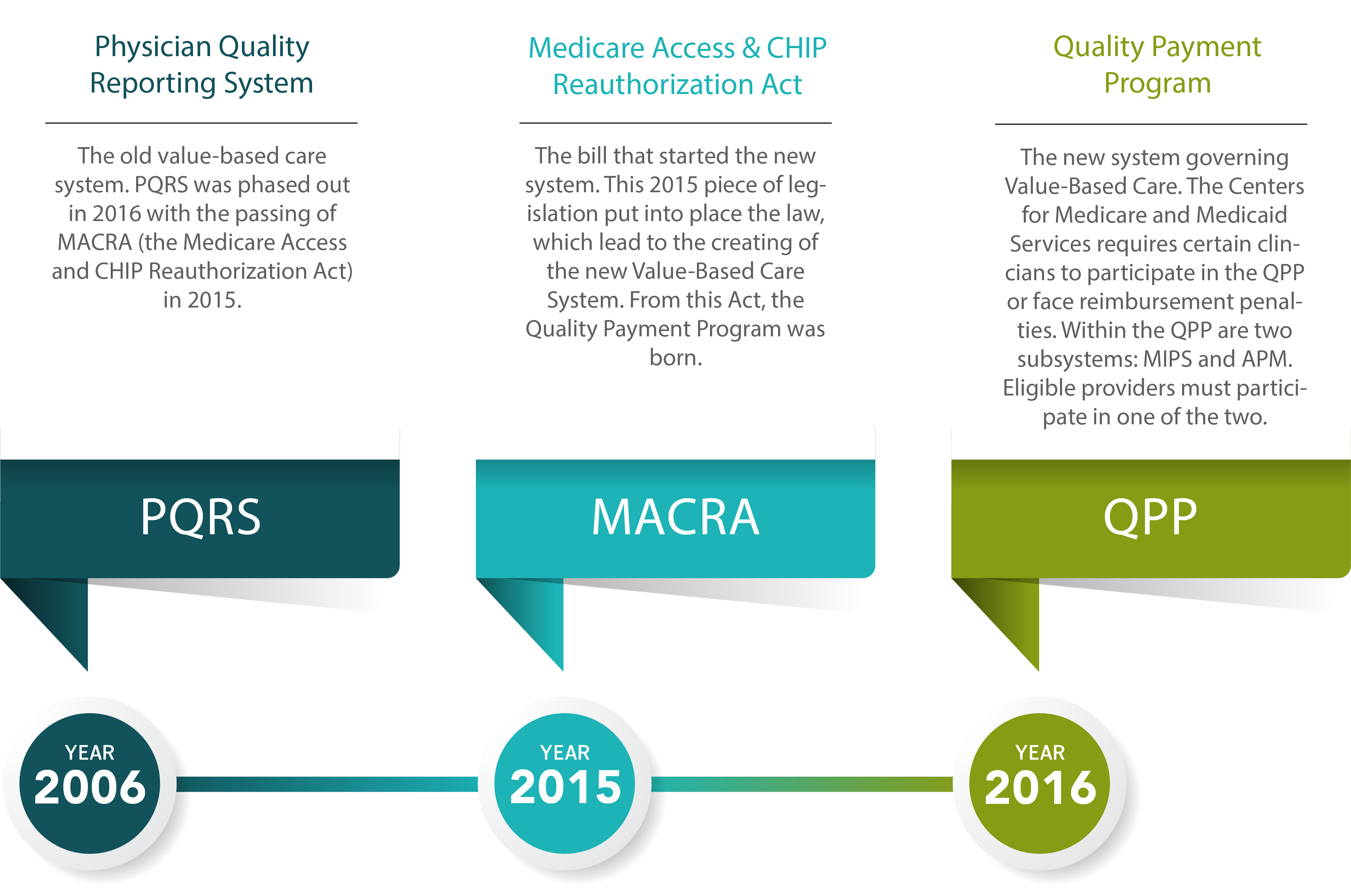
Text Version of Above Value-Based Care Timeline
2006
PQRS
Physician Quality Reporting System
The old value-based care system. PQRS was phased out in 2016 with the passing of MACRA (the Medicare Access and CHIP Reauthorization Act) in 2015.
2015
MACRA
Medicare Access & CHIP Reauthorization Act
The bill that started the new system. This 2015 piece of legislation put into place the law, which lead to the creating of the new Value-Based Care System. From this Act, the Quality Payment Program was born.
2016
QPP
Quality Payment Program
The new system governing Value-Based Care. The Centers for Medicare and Medicaid Services requires certain clincians to participate in the QPP or face reimbursement penalties. Within the QPP are two subsystems: MIPS and APM. Eligible providers must participate in one of the two.
The Two QPP Reporting Options
MIPS and APMs
MIPS
Merit-based Incentive Payment System
MIPS combines parts of various old value-based care system into one new program, in which Eligible Clinicians are measured on four specific performance categories:
- Quality (replaced PQRS)
- Improvement Activities (new category)
- Promoting Interoperability (replaced Meaningful Use)
- Cost (replaced Value-Based Payment Modifier)
For 2020 and 2021, clinicians who bill $90,000 or more in Medicare Part B allowed charges, see more than 200 Part B-enrolled Medicare beneficiaries, and provide 200 or more covered professional services to Part B Medicare patients are eligible for MIPS. Such eligible providers must participate or face reimbursement penalties.
APMs
Alternative Payment Models
Alternative Payment Models essentially allow for more extensive participation in the transition to Value-Based Care. As of 2019, advanced APM participation requires providers to either a) receive 50 percent of their Medicare Part B payments through an Advanced APM, OR b) see 35 percent of their Medicare patients through an Advanced APM.
Participation is strictly voluntary and reserved to providers (both MIPS-eligible and not) who meet certain requirements. Such participating clinicians are eligible to receive larger reimbursement incentives, while potentially taking on greater financial risk as well.
APM options are designed by the CMS, with the goal of strengthening specific aspects or fields of medical care. Participating physicians contribute valuable data, which helps the CMS shape evaluation standards. APMs apply to a specific clinical condition, a care episode, or a population.